Over the past few decades, dietary advice around the world was dominated by one simple mantra: cut fat, eat more carbohydrates, and count calories. We now know that this approach didn’t work.
Across countries especially in the U.S. and India, chronic diseases like obesity, type 2 diabetes, fatty liver, heart disease and metabolic syndrome have skyrocketed. These are not simply “lifestyle choices” in isolation; they are metabolic consequences of how food affects hormones like insulin.
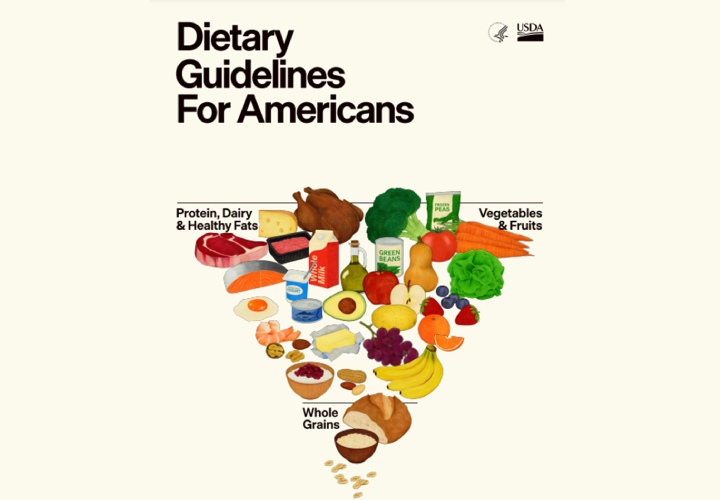
In early January 2026, the United States issued its 2025–2030 Dietary Guidelines, marking a bold rethinking: the focus is now on real food, not calorie counting or macronutrient percentages alone.
This shift aligns closely with what many clinicians call a Low-Carb, Healthy-Fat (LCHF) approach and it offers powerful lessons for India’s own dietary policies amid its NCD crisis.
What the New U.S. Dietary Guidelines Say (and Why It’s Important)
The 2025–2030 Dietary Guidelines for Americans emphasize:
- Whole, minimally processed foods
- Reduced added sugars (no amount is “healthy”)
- Higher protein intake around 1.2–1.6 g per kg of body weight
- Healthy fats allowed, with moderation on saturated fat
- Lower refined carbohydrates
- De-emphasis on ultra-processed foods that dominate modern diets
This is a paradigm shift from past guidelines that promoted high carbohydrate and low-fat eating.
Key points that resonate with an LCHF view:
- Carbohydrates are not inherently “healthy” quality and quantity matters.
- Added sugars and refined starches disrupt insulin regulation.
- Healthy fats and adequate protein support metabolic health.
While not labeled LCHF, the U.S. guidance indirectly validates principles widely used in metabolic clinics: less refined carbs + high-quality protein + healthy fats = better insulin control and metabolic outcomes.
India’s NCD Crisis: The Clinical Reality
India is in the midst of a noncommunicable disease (NCD) epidemic and diet is a central driver along with lifestyle.
Alarming Clinical Data
- Diabetes: Around 101 million Indians currently have diabetes (≈11.4 % of adults), and 136 million are pre-diabetic.
- Hypertension: A staggering 315 million have high blood pressure.
- Generalized Obesity: Affects around 254 million people.
- Abdominal Obesity: Around 351 million Indians have excessive central fat, a strong risk factor for metabolic disease.
- High cholesterol and LDL: Widespread dyslipidemia further increases heart disease risk.
- 56 % of India’s disease burden is linked to unhealthy diets according to ICMR nutritional insights.
These numbers show NCDs are not rare diseases but they are mainstream public health emergencies.
The Connection: Diet, Insulin, and Metabolic Disease
At the root of this epidemic is chronically elevated insulin, driven by diets high in refined carbohydrates and added sugars and not by healthy fats.
This is exactly where LCHF makes sense:
- Refined carbs quickly spike blood glucose, triggering high insulin and insulin resistance.
- High insulin levels drive fat storage, hunger, and chronic inflammation.
- Reducing carb load improves insulin sensitivity, which is the core objective of LCHF.
An Indian Council of Medical Research (ICMR) study highlighted that many Indians eat ~62 % of calories from carbohydrates, often from poor-quality sources like white rice and refined wheat, while protein intake is critically low (~12 %) and intake of healthier fats is suboptimal.
This imbalance is statistically linked to higher risks of diabetes, prediabetes, obesity and abdominal obesity in epidemiological analysis.
How India Can Adapt the U.S. Shift — With LCHF in Mind
India doesn’t need to replicate U.S. policy as every culture has unique foodways but, the principles are universal.
1. Reduce Refined Carbohydrates and Added Sugars
Instead of:
- Unlimited rice and wheat
- Sugary snacks, sweetened tea, packaged snacks
Move toward:
- Lower overall carb portions
- Increased vegetables, legumes, and fiber
- Curbing sugar as a non-essential ingredient
This aligns with U.S. advice to limit added sugars and with LCHF emphasis on metabolic impact rather than calories.
2. Prioritize Protein and Healthy Fats
India’s predominantly high-carb plates often lack adequate protein.
Clinical data suggests:
- Higher protein improves satiety.
- Better preserves muscle mass with age.
- Lowers post-meal glucose excursions.
Healthy fats (like ghee, mustard, nuts, seeds, dairy) should not be feared, they help regulate appetite and support metabolic health when used judiciously.
3. Re-Balance Macronutrients — Quality Over Quantity
Instead of:
- 60–70 % calories from refined carbs
- Few proteins and limited healthy fats
Consider:
- Moderate carbohydrate intake focused on whole sources
- Adequate protein daily; aim toward 1.2 g/kg/day as the U.S. guidance suggests
- Healthy fats for satiety and micronutrient delivery
These changes reduce insulin surges and may help reverse metabolic dysfunction.
4. Align Policies with Metabolic Outcomes
Dietary guidelines should:
- Limit sugar and ultra-processed foods
- Promote accessible protein sources (pulses, dairy, eggs, fish)
- Encourage traditional nutrient-dense foods (millets, legumes, greens)
Remember: diet quality influences disease risk more than calorie counts alone.
Towards a Healthier Future: Integrating Science with Culture
The U.S. shift toward real foods, less refined carbs, and emphasis on protein and healthy fats is not a fad, it reflects emerging evidence on how diets influence metabolism and disease risk.
India’s clinical reality is the soaring diabetes, obesity, hypertension, dyslipidemia. It demands a similarly evidence-based overhaul of dietary guidance. Combining the core logic of LCHF with culturally relevant foods could help millions prevent, manage, or even reverse metabolic diseases.
Because health isn’t just about avoiding disease — it’s about designing food systems, guidelines, and habits that support thriving lives.
Image credit: realfood.gov

Leave a Reply